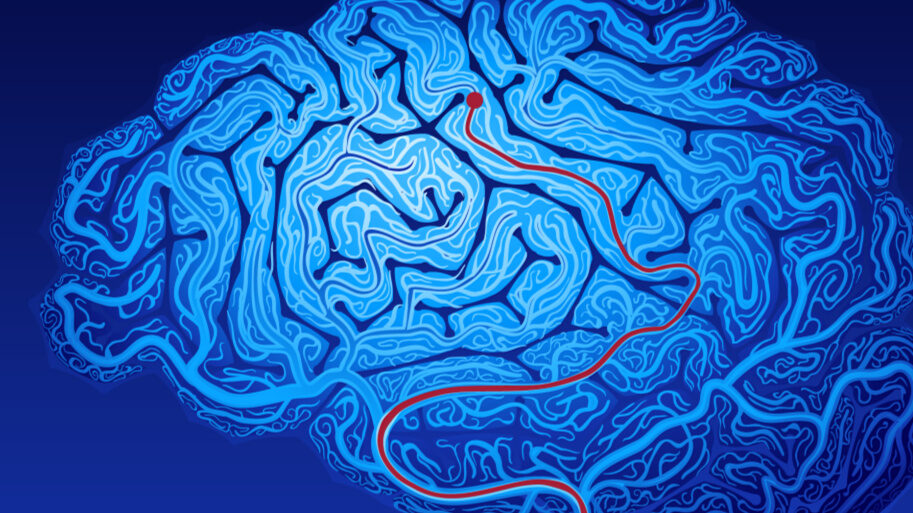
In the fast-evolving realm of emergency medical services (EMS), pre-hospital stroke care represents a crucial frontier. As paramedics and emergency medical technicians (EMTs), you hold the pivotal responsibility of influencing patient outcomes long before they reach the hospital. This blog post delves into the nuts and bolts of pre-hospital stroke care, highlighting key assessments and interventions that can significantly alter patient prognosis.
The Essentials of Neuroassessment
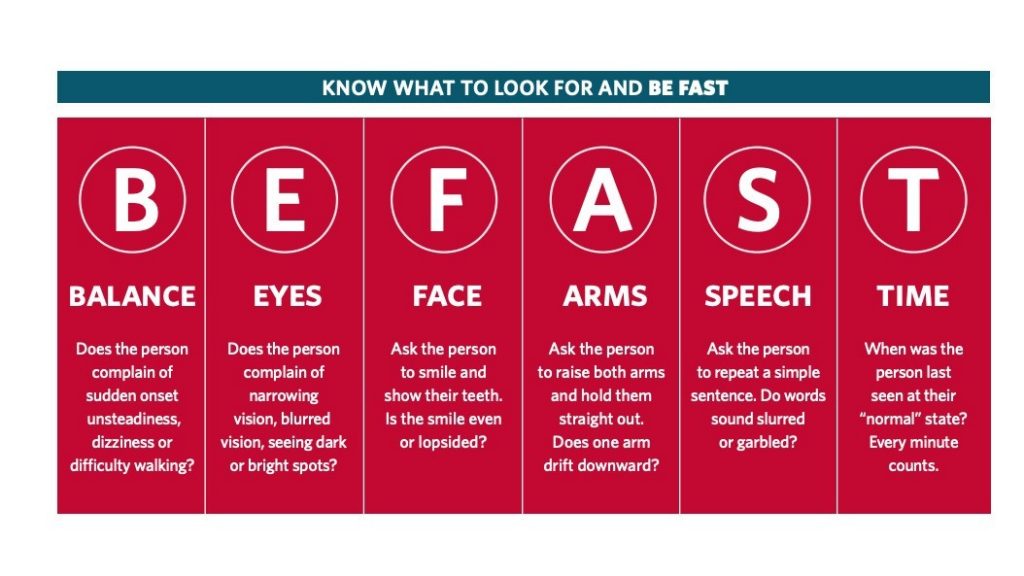
A competent and consistent neuroassessment forms the cornerstone of effective pre-hospital stroke care. Adopting a reliable neuroassessment protocol ensures that you can accurately identify strokes—even those with atypical presentations. One practical tool is the BEFAST acronym:
- Balance: Assess the patient’s ability to walk. Difficulty in ambulation is a strong indicator of a stroke.
- Eyes: Look for nystagmus (rapid involuntary eye movement), though challenging to detect in the field. Assess extraocular movements and identify any double vision, especially if it worsens at extremes of vision and resolves with closing one eye. Assess visual acuity in all four quadrants of each eye.
- Face: Check for facial droop or asymmetry.
- Arms: Look for arm drift or unilateral weakness.
- Speech: Evaluate for slurred speech or difficulty in speaking.
- Time: Determine the last known well time, a critical factor for subsequent therapy.
Paramount Interventions in Stroke Care
Once a stroke is suspected, several interventions can streamline the transition to definitive care:
- Pre-notification: Inform the receiving facility about the stroke suspicion, enabling them to prepare in advance. Pre-notification can significantly reduce time to critical interventions like CT scans and administration of thrombolytics.
- Last Known Well: Establish and document the last known normal time. This information is vital for determining eligibility for thrombolytics (e.g., TPA).
- Blood Glucose Check: Quickly rule out hypoglycemia, as it can mimic stroke symptoms.
- IV Access: Secure a 20-gauge or larger IV, preferably in the arm, to facilitate rapid administration of medications and contrast for imaging.
Knowing Your Stroke Centers
Awareness of the capabilities of nearby stroke centers is crucial. The American Heart Association (AHA) provides guidelines categorizing stroke centers that paramedics should be familiar with:
- Comprehensive Stroke Centers: Equipped for 24/7 mechanical thrombectomy and extensive care.
- Thrombectomy-Capable Stroke Centers: Can perform thrombectomy but may not offer round-the-clock coverage.
- Primary Stroke Centers: Capable of administering TPA but will transfer patients needing more extensive care.
- Acute Stroke Ready Hospitals: Have basic infrastructure for acute stroke care but will also transfer complex cases.
When deciding which facility to transport a stroke patient to, drive time is a critical factor:
- In urban areas, transport patients to a comprehensive stroke center within 30 minutes, even if it means bypassing other facilities.
- In suburban areas, this window extends to 45 minutes, and in rural areas, to 60 minutes.
However, only 20% of patients aged 55 and over in the U.S. live within 15 to 30 minutes of a primary stroke center, highlighting the importance of rapid prehospital assessment and transport decisions.
Transport decisions augment the complexity of pre-hospital stroke care. With variable guidelines and ever-evolving protocols, it’s imperative to stay informed and make judicious choices. When faced with the decision, consider the drive times to various centers and their capabilities. Local protocols will often guide these choices, but having a solid understanding ensures you can advocate for the best patient care.
The Power of Timely and Accurate Care
The implications of timely and accurate stroke care extend far beyond initial transport. Research highlights the correlation between efficient pre-hospital interventions and improved patient outcomes. Metrics such as time to CT scan, time to TPA administration, and overall neurological functions upon discharge are impacted by the care you provide prior to the arrival to the hospital.
Key Prehospital Interventions
The American Heart Association (AHA) outlines eight critical tasks for paramedics when managing a suspected stroke patient. However, research indicates that not all these interventions consistently improve outcomes. Prioritizing the following tasks can significantly impact neurologic outcomes by reducing time to CT:
- Neuro Assessment:
- Conduct a thorough neuro exam to identify focal deficits.
- Last Known Normal Time:
- Document the exact time the patient was last seen normal to determine treatment windows.
- Blood Glucose Level (BGL):
- Check BGL to rule out hypoglycemia as a cause of symptoms.
- Pre-Notification:
- Alert the receiving hospital about the incoming stroke patient to expedite preparations.
Conclusion
For today’s EMS providers, excellence in pre-hospital stroke care means mastering quick, accurate assessments and effective interventions. It’s about being prepared to execute fundamental tasks that are proven to impact patient outcomes. As you head out for your next shift, let the pillars of BEFAST and awareness of your transport options guide you. Remember, in the world of stroke care, every second saved can translate into millions of neurons preserved.
Stay tuned for updates on the latest research and evolving guidelines to ensure that your practice remains at the cutting edge of EMS stroke care. As always, your role is vital and your impact, immeasurable. Thank you for your continued dedication to enhancing patient outcomes in the most critical moments.