Welcome to the world of neonatal resuscitation, a realm where quick thinking and decisive action are essential. In this episode of EMS cast, Dr. Avery MacKenzie, an ER physician in Southwest Colorado, shares her experiences and insights into neonatal resuscitation. As a rural healthcare provider, she faced the challenge head-on, conquering her fears to become proficient in handling these critical situations. In this blog post, we’ll delve into the key points discussed in the podcast, providing valuable information for emergency providers on the streets.
Understanding the Fear:
Neonatal resuscitation may seem daunting, especially when faced with unexpected situations in the middle of the night. Dr. MacKenzie emphasizes that while it might be scary, it’s not inherently difficult. The key is to recognize that as a healthcare provider, you possess the skills needed to navigate through the process. By overcoming the initial fear and focusing on your training, you can confidently approach neonatal resuscitation.
Dr. McKenzie’s Journey:
As a rural nocturnist, Dr. MacKenzie identified neonatal resuscitation as one of her greatest fears. To address this, she decided to delve into the topic, giving lectures and staying updated on the latest techniques. Her proactive approach not only helped her conquer her fears but also equipped her to handle neonatal resuscitations effectively in real-life scenarios.
Real-Life Scenario: Pre-hospital Outborne Delivery
Dr. MacKenzie recounts a challenging pre-hospital delivery scenario during a snowstorm, where a 30-week premature baby was born before reaching the hospital. The podcast discusses the critical steps taken in this situation.
Key Steps in Neonatal Resuscitation:
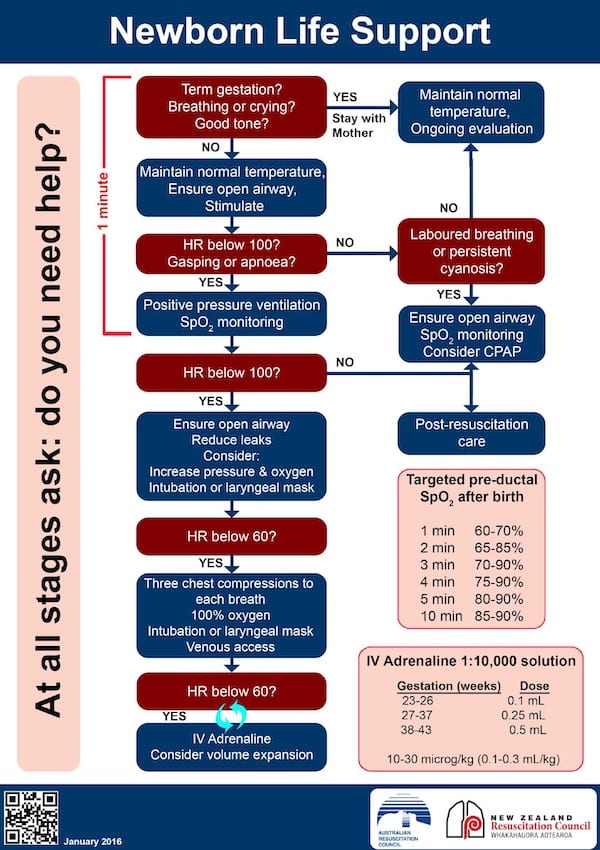
Initial Assessment
- Check gestational age (term or preterm).
- Assess muscle tone and respiratory effort.
- Determine if the baby needs resuscitation based on the three questions: term gestation, good tone, and good respiratory effort. If the answer is yes to all of three of these, give baby to mom for skin to skin contact. If the answer is no to any of these three questions, take baby and start resuscitation as follows.
First 30 Seconds:
- Warm, dry, stimulate, and position the airway.
- Assess respiratory effort and heart rate.
Positive Pressure Ventilation:
- Initiate if heart rate is below 100 or if the baby is apneic or gasping.
- Maintain a rate of 40 to 60 breaths per minute.
Assess Progress:
- Continuously monitor heart rate to gauge the effectiveness of resuscitation.
- If heart rate improves to over 100, transition to post-resuscitation care.
- If heart rate does not improve to over 100, improve your ventilations.
Improving Ventilation:
- Use the “MR. SOPA” mnemonic: Mask adjustment, Repositioning airway, Suctioning, Opening mouth, Increasing pressure, and consider an Advance airway.
If Heart Rate Remains or Drops Below 60 Despite Positive Pressure Ventilation:
- Initiate coordinated chest compressions and ventilations (3:1 ratio).
- Consider advanced airway options, but prioritize effective ventilation.
Advanced Airway Considerations:
In the pre-hospital setting, the emphasis is on providing high-quality bag-valve-mask (BVM) ventilations. The use of advanced airways, such as intubation, is de-emphasized due to the challenging nature of the procedure and the potential for interruptions in ventilation. Supraglottic airways, such as the i-gel, may be considered for infants 34 weeks or greater.
Conclusion:
Neonatal resuscitation requires a combination of knowledge, confidence, and the ability to adapt to challenging situations. As emergency providers, embracing the fear and acquiring the necessary skills will enable you to make a significant impact during neonatal resuscitations, ensuring the best possible outcomes for these tiny lives.
Other Resources: