What is the ACS?
It is important to listen to experts in the field, and the American College of Surgeons (ACS) is a great example of a group of experts that can provide valuable insight. The ACS is a national group of physicians that come together to determine best practices and guidelines for surgery, especially trauma surgery. They look at the evidence, consider different perspectives, and come up with the best guidelines. When making recommendations they will point to the evidence and rank it based on its quality and strength, such as double-blind randomized controlled placebo trials. If there is no evidence at all, they use expert consensus to come up with the best guidelines.
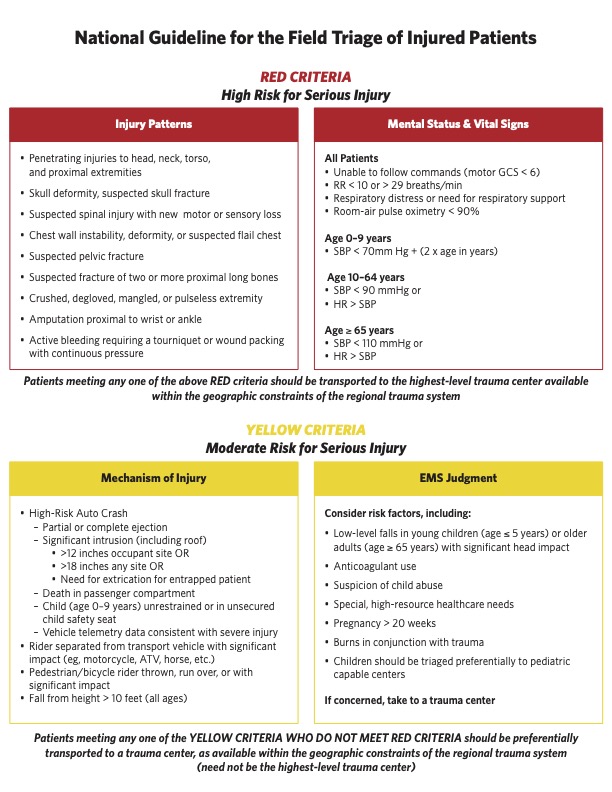
The ACS recently revised their guidelines for field trauma triage and took a different approach than the traditional algorithm. Instead of a prescriptive, “if-then” model, they created lists of criteria that indicate a patient is red or yellow. This principle-based approach is more effective and can help us better assess and triage patients.
These new ACS recommendations can help us make the best decisions in the field and provide quality care to our patients. They provide valuable insight and guidance that can help us in our daily work. It is important to stay up to date with the latest guidelines and recommendations from the ACS so that we can best serve our patients.
The Update
Simplify trauma triage.
One of the most important aspects of providing quality care is being able to quickly and accurately triage patients in the field. This is especially important in a multiple casualty incident (MCI) situation, where time is of the essence and decisions need to be made quickly. The ACS has recently updated their trauma triage guidelines, which they hope will help simplify the process.
The new guidelines are designed to make triage easier and more efficient by removing the cognitive burden from the pre-hospital providers. Instead of relying on algorithms or complex acronyms, the new guidelines focus on quickly assessing the patient’s condition and providing the appropriate level of care. The guidelines also encourage pre-hospital providers to think critically and practice their understanding of pathophysiology. This helps them to make informed decisions about the best course of action for each patient.
The new guidelines also emphasize the importance of quickly assessing the patient’s condition and providing the appropriate level of care. Instead of trying to categorize all of the patients, the guidelines suggest that providers should focus on the reds and yellows and let the greens take care of themselves. This helps to reduce the cognitive burden and ensure that resources are being used efficiently.
Overall, the new guidelines from the ACS are designed to simplify trauma triage and make it easier for pre-hospital providers to quickly and accurately assess and treat patients in the field. By removing the cognitive burden and encouraging providers to think critically and practice their understanding of pathophysiology, the new guidelines can help to ensure that resources are being used efficiently and that patients are receiving the best possible care.
Develop clinical acumen.
Developing clinical acumen is essential for pre-hospital providers in order to provide the best care for their patients. Clinical acumen is the ability to quickly and accurately assess and treat patients in the field. It is the ability to think critically and to recognize patterns in patient presentations. It is also important to be able to recognize when a patient does not fit the typical pattern and to be able to adjust the treatment accordingly.
Developing clinical acumen requires practice and experience. Pre-hospital providers should take every opportunity to practice their skills and to learn from their mistakes. One way to do this is to take time to feel the radial pulse of every patient. This can help to give an indication of the patient’s heart rate, strength, and regularity. It also gives providers an opportunity to practice their physical assessment skills.
Pre-hospital providers should also take time to review after-action reports of multi-patient calls. This can help to provide a better understanding of how to identify and treat patients in a variety of situations. It is also important to read and understand the guidelines from the American College of Surgeons. This will ensure that providers are following the most up-to-date protocols and that they are using their resources efficiently.
Developing clinical acumen is essential for pre-hospital providers in order to provide the best care for their patients. It is important to take time to practice physical assessment skills, to review after-action reports, and to understand the guidelines from the American College of Surgeons. By doing these things, pre-hospital providers can ensure that they are prepared to handle any situation they may encounter and that they are providing the best possible care for their patients.
Assess body systems quickly.
One of the most important skills for pre-hospital providers is the ability to quickly assess body systems. This is especially important in emergency situations, where seconds can mean the difference between life and death. The American College of Surgeons has determined that only four body systems can lead to immediate death if they fail: the neurologic system, the respiratory system, the cardiovascular system, and the hematologic system. If any of these four systems fail, it is essential that pre-hospital providers are able to quickly assess the patient and determine the best course of action.
One way to quickly assess body systems is to feel for a pulse. This can be done as part of a handshake, and can provide valuable information about the patient’s cardiovascular system. In addition, pre-hospital providers should assess the patient’s ability to follow commands, their respiratory effort, and any gross blood loss. This assessment should be done on every call, regardless of whether it is an emergent or non-emergent response.
Pre-hospital providers should also be aware of the signs and symptoms of neurologic system failure. These can include difficulty tracking movements, slurred speech, and difficulty answering questions. By being aware of these signs and symptoms, pre-hospital providers can quickly assess the neurologic system and determine the best course of action.
In conclusion, pre-hospital providers must be able to quickly assess body systems in order to provide the best possible care for their patients. This is especially important in emergency situations, where seconds can mean the difference between life and death. Pre-hospital providers should be aware of the guidelines from the American College of Surgeons, and should practice physical assessment skills in order to be prepared to handle any situation they may encounter.
Assess age, comorbidities, vitals.
When it comes to assessing a patient in a pre-hospital setting, there are a few key elements that must be taken into consideration. One of the most important elements is to assess age, comorbidities, and vitals. Age and comorbidities can help provide insight into a patient’s overall health status, while vitals can help provide a baseline for the patient’s current condition.
When assessing age, pre-hospital providers should be aware of the general guidelines from the American College of Surgeons. These guidelines suggest that patients over the age of 65 should be considered a higher priority for care. Additionally, pre-hospital providers should be aware of any comorbidities that a patient may have. Comorbidities can include conditions such as diabetes, heart disease, or hypertension. Knowing these conditions can help pre-hospital providers better understand the patient’s overall health status and prioritize care accordingly.
Finally, pre-hospital providers should assess the patient’s vitals. This includes taking the patient’s temperature, blood pressure, pulse, and oxygen saturation. These vitals can provide a baseline for the patient’s condition and can help pre-hospital providers determine if the patient is in need of immediate care or can wait for transport to a hospital.
Assessing age, comorbidities, and vitals is an essential part of providing pre-hospital care. Pre-hospital providers should be aware of the American College of Surgeons guidelines and should practice physical assessment skills in order to be prepared to handle any situation they may encounter. By assessing these elements, pre-hospital providers can provide the best possible care for their patients.
Deliberate repetition yields growth.
Deliberate repetition yields growth in the pre-hospital setting. Pre-hospital providers must practice physical assessment skills in order to be prepared for any situation they may encounter. This repetition helps to build the skills necessary to quickly and accurately assess a patient’s condition. By repeating the same assessment steps over and over, pre-hospital providers can become more adept at recognizing subtle changes in a patient’s condition.
The pre-hospital provider must also be aware of the American College of Surgeons guidelines for pre-hospital care. This includes assessing age, comorbidities, and vital signs. By being familiar with these guidelines, pre-hospital providers can quickly identify the most important factors to consider when assessing a patient. Additionally, they can determine the best course of action for each patient.
The pre-hospital provider must also take into account the patient’s environment and other factors. This includes looking at the patient’s skin color, eyes, response to movements, and response to questions. By taking these elements into account, pre-hospital providers can quickly assess the patient’s condition and determine if they are sick or not.
In addition to assessing the patient’s condition, pre-hospital providers must also consider the patient’s risk factors and medical history. This helps to ensure that the provider is providing the best possible care for the patient. By taking into account these elements, pre-hospital providers can better prepare for any situation they may encounter.
Deliberate repetition is essential for pre-hospital providers. By repeating the same assessment steps over and over, pre-hospital providers can become more adept at quickly and accurately assessing a patient’s condition. Additionally, by being familiar with the American College of Surgeons guidelines and considering the patient’s environment and risk factors, pre-hospital providers can provide the best possible care for their patients.
Practice system one thinking.
System one thinking is a term used to describe the cognitive process of making quick decisions based on past experiences. System one thinking is automatic and requires little effort, allowing pre-hospital providers to make decisions quickly and efficiently. System one thinking is especially important in pre-hospital care because of the often chaotic and unpredictable nature of emergency situations. Pre-hospital providers need to be able to make decisions quickly and accurately, and system one thinking allows them to do so.
System one thinking is not only important for pre-hospital providers, but it is also important for all healthcare providers. System one thinking can help healthcare providers make decisions quickly and accurately in a variety of situations. For example, a healthcare provider may need to make a decision about which patient to prioritize first or which treatment to use in a particular situation. By being familiar with the patient’s history and the current situation, healthcare providers can make decisions quickly and accurately using system one thinking.
System one thinking is essential for pre-hospital providers. By practicing system one thinking, pre-hospital providers can make decisions quickly and accurately in emergency situations. Additionally, system one thinking can help healthcare providers make decisions quickly and accurately in a variety of situations. Pre-hospital providers should strive to practice system one thinking in order to provide the best possible care for their patients.
Trust your gut.
One way that pre-hospital providers can practice system one thinking is by trusting their gut. In the podcast, the speaker emphasizes the importance of “honing your gut” and trusting it. This is a reference to system one thinking, which relies on intuition and instinct. System one thinking allows pre-hospital providers to make decisions quickly and accurately in a variety of situations.
In the podcast, the speaker gives several examples of when pre-hospital providers should trust their gut. For example, if a patient has been ejected from a vehicle, the pre-hospital provider should trust their gut and prioritize that patient for transport to the trauma center. Additionally, if a pre-hospital provider is evaluating two patients and one of them is on anticoagulants, the pre-hospital provider should trust their gut and prioritize that patient for transport. Finally, if a pre-hospital provider is concerned about a patient, they should trust their gut and transport the patient to a trauma center.
Trust your gut is an important skill for pre-hospital providers to practice. System one thinking is essential for pre-hospital providers, as it allows them to make decisions quickly and accurately in a variety of situations. Pre-hospital providers should strive to practice system one thinking, and trust their gut, in order to provide the best possible care for their patients.
Trust your gut, over-triage.
One of the most important aspects of pre-hospital care is the ability to trust your gut and make decisions quickly. Pre-hospital providers are often faced with complex situations that require them to make decisions quickly and accurately. System one thinking is a form of thinking that allows pre-hospital providers to make decisions quickly and accurately, without having to spend too much time analyzing the situation. System one thinking involves trusting your gut and making decisions based on your intuition and experience.
Trust your gut and over-triage is an important concept for pre-hospital providers to understand. Over-triage is the practice of sending more patients to a higher-level care facility than is necessary. This practice is encouraged by the American College of Surgeons (ACS) guidelines, which suggest that a certain margin of over-triage is beneficial and should be practiced. The reason for this is that it is better to err on the side of caution and send a patient to a higher level of care than to not send them at all.
Pre-hospital providers should strive to practice system one thinking and trust their gut when making decisions. This is especially important in situations where there are multiple patients and the provider must make decisions quickly. In these situations, it is important for the provider to consider all the factors and make decisions based on their experience and intuition. Additionally, pre-hospital providers should strive to practice over-triage in order to ensure that their patients receive the highest level of care possible.
Overall, trust your gut and over-triage is an important concept for pre-hospital providers to understand and practice. System one thinking is essential for pre-hospital providers, as it allows them to make decisions quickly and accurately in a variety of situations. Pre-hospital providers should strive to practice system one thinking, and trust their gut, in order to provide the best possible care for their patients. Additionally, pre-hospital providers should strive to practice over-triage in order to ensure that their patients receive the highest level of care possible.
Practice quick physical exams.
One of the most important concepts for pre-hospital providers to understand is the importance of system one thinking and trust your gut. System one thinking is the ability to make quick decisions in a variety of situations. This type of thinking is essential for pre-hospital providers, as it allows them to make decisions quickly and accurately in a variety of situations. Pre-hospital providers should strive to practice system one thinking in order to provide the best possible care for their patients.
Another important concept for pre-hospital providers to understand is the importance of over-triage. Over-triage is the practice of providing the highest level of care possible to a patient, regardless of the severity of their condition. This practice is essential for pre-hospital providers, as it ensures that their patients receive the highest level of care possible. Pre-hospital providers should strive to practice over-triage in order to ensure that their patients receive the highest level of care possible.
Finally, pre-hospital providers should strive to practice quick physical exams. A quick physical exam is a type of exam that is conducted in the first five seconds of any patient interaction. This type of exam allows pre-hospital providers to look for key indicators of injury, some of which can be subtle. Pre-hospital providers should strive to practice quick physical exams on every single call, in order to ensure that they are able to identify and treat potential injuries as quickly as possible.
In conclusion, pre-hospital providers should strive to practice system one thinking, trust their gut, and practice over-triage in order to provide the best possible care for their patients. Additionally, pre-hospital providers should strive to practice quick physical exams in order to ensure that they are able to identify and treat potential injuries as quickly as possible. By practicing these concepts, pre-hospital providers can ensure that their patients receive the highest level of care possible.