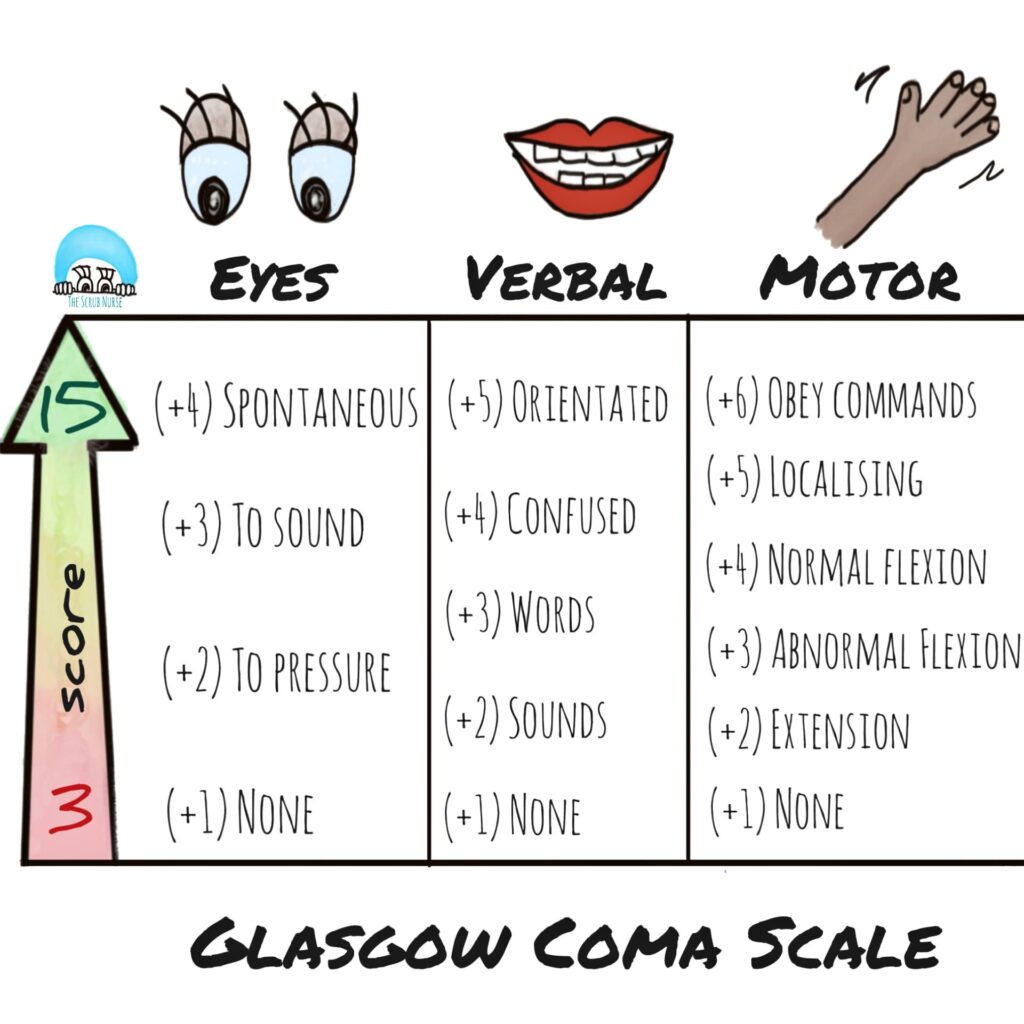
The Glasgow Coma Score (GCS) was developed in the 1970s initially as a research tool for admitted Neurosurgery patients. The original authors of the score and research advocated against it’s widespread use in acute care but nevertheless here we are: it is widely used in acute trauma and medical care. Other than a score of 3 or a score of 15, there are multiple combinations of numbers that can get you various scores. This results in a poor ability to know what the patient is actually doing. The same combined score can represent two very different patients making the score difficult to interpret:
| Patient 1GCS = 10 | Patient 2GCS = 10 | |
| Eyes | 4 = spontaneous | 2 = open to pain |
| Verbal | 5 = oriented | 3 = inappropriate words |
| Motor | 1 = No response | 5 = localizes to pain |
Which patient above are you more worried about? There is some rationale to use GCS as triage tool for trauma center vs not:GCS <13 –> level 1 (or highest available trauma center in your system)GCS > 13 –> can go to lower level trauma center (if they don’t otherwise meet other system criteria for a level 1 trauma center) In fact the most recent American College of Surgeons (the major trauma surgery body in the USA) field triage criteria have moved on to using a motor-GCS or M-GCS only:M-GCS <6 –> level 1 (or highest available trauma center in your system)M-GCS = 6 –> can go to lower level trauma center (if they don’t otherwise meet other system criteria for a level 1 trauma center):
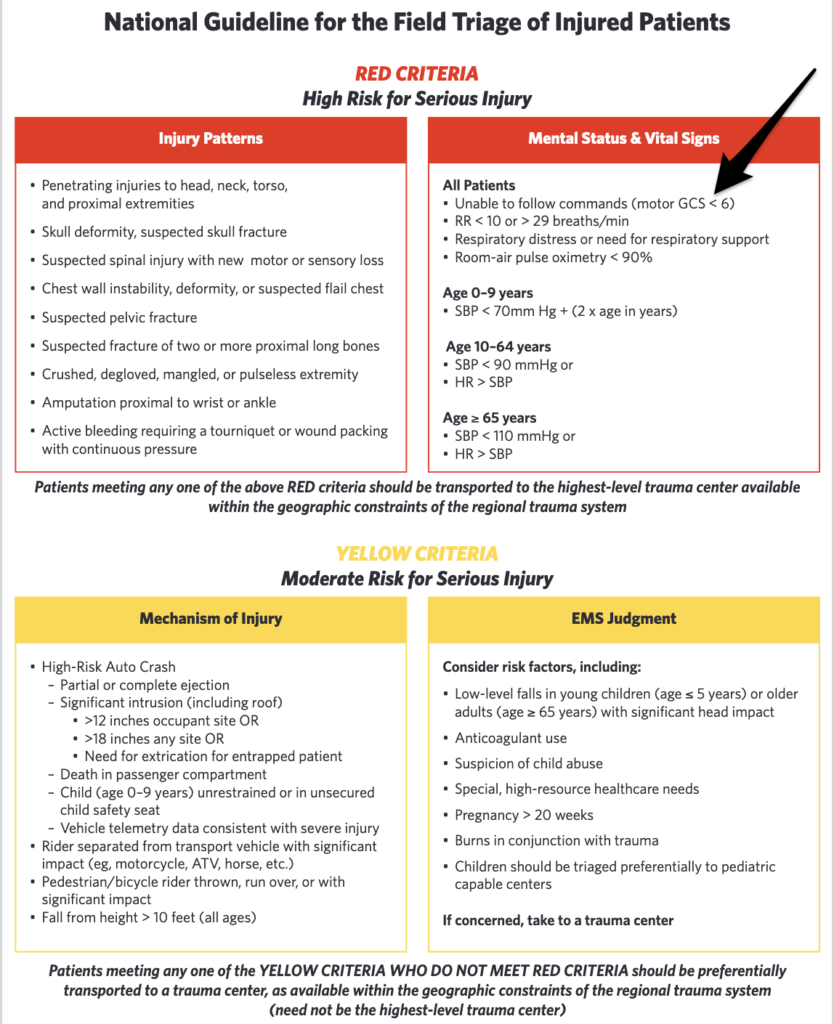
Source: https://www.facs.org/quality-programs/trauma/systems/field-triage-guidelines/
Another score or called the Simplified Motor Score is something that is out there but it is pretty complex and not worth committing to memory. Stick to either total GCS or M-GCS.
With all of the above out of the way, the best thing to do is to be honest. The GCS is just trying to capture the exam in the form of a number. It’s hard to do math when you’re stressed. It’s much easier to describe what you are seeing. One example of this is to use the AVPU scale plus a qualifier if needed (eg Responds to pain but heavily intoxicated or status post sedation etc)
If your system loves the GCS and wants the GCS you just have to try to do the GCS. If you know they aren’t following commands and you use that information to transport to the highest available trauma center, you wont under triage or do wrong by the patient. End of the day be honest: “I’m having a hard time doing the math in the heat of the moment but here is what I’m seeing.”
Bottom Line:
- Not following commands = go to the highest level trauma center available to you in your system
- GCS is not that great but your system may love it
- What the GCS is trying to capture is a neurological exam in the trauma patient. This is what is important.
- Communicate the same information in an honest way that will get the pt the care they need.