Syncope, is a symptom that many emergency medical personnel encounter. It’s sometimes tricky to differentiate from seizures, and it’s essential to understand that syncope is not a standalone diagnosis. It’s a symptom of an underlying cause, which can be benign or life-threatening. Let’s delve into the world of syncope, explore its clinical significance, and discuss how EMS providers can effectively assess and risk stratify patients who experience it.
Why Is Syncope Important?
Syncope is a frequent call for EMS providers, and while it often results from minor issues like dehydration or a vasovagal reaction, it can also signal a critical, life-threatening problem. The challenge lies in determining when syncope is a benign episode or when it requires urgent intervention.
The Guiding Principles of Syncope
Every syncope or near syncope patient requires 3 things-
- Careful history-taking regarding the current and previous episodes (including eyewitness accounts) and any symptoms that occurred surrounding the event
- Every patient needs a physical exam that includes heart sounds, lung sounds, abdominal exam, lower extremity exam, and a complete neurologic exam
- Every patient needs an EKG, looking for arrhythmia or secondary signs of arrhythmia
The goal is to risk stratify the syncope into low or high risk. Realize that individuals who experience near syncope have the exact same risk and outcomes as those who experienced a syncope.
Syncope in EMS Practice
The Initial Approach
When responding to a syncope call, the first step is setting the stage for a proper assessment. Ensure the patient is seated or in a comfortable position for evaluation. Often, patients are found on the floor, surrounded by concerned bystanders. Move them, if possible, to an area where you can conduct a thorough assessment, including taking a history, performing a physical examination, and obtaining an EKG.
Differentiating from Seizures
One of the complexities in assessing syncope is distinguishing it from seizures. Some syncope episodes may include movements resembling seizure activity, known as myoclonic jerks. Two primary indicators help in differentiation: how rapidly the patient returns to baseline and the presence of tongue biting. If there is a period of confusion following the loss of consciousness and/or if the patient has evidence of cheek or tongue biting these are usually more indicative of a seizure. Syncope should present with a sudden loss of consciousness and a rapid return to baseline.
Understanding the Causes and Symptoms
Low, Medium, and High-Risk Indicators
- Low-Risk Syncope: Often associated with vasovagal episodes or dehydration. Characterized by classic symptoms such as nausea, tunnel vision, and feeling flushed before fainting. It’s generally benign, especially if there are no additional concerning symptoms.
- High-Risk Syncope: Identified by the presence of syncope plus another high risk symptom (e.g., chest pain, shortness of breath, lower extremity pain/swelling, abdominal pain, headache, or focal neurological deficits). These patients may have serious underlying conditions such as PE, ectopic pregnancy, aortic disection/aneurysm, or subarachnoid hemorrhage. The physical exam and EKG are also very important, any presence of a murmur or abnormal finding on EKG (see below) will also place a syncope patient into the high risk category.
- Medium-Risk Syncope: Where the cause is unclear and there’s no prodromal symptom (i.e. no warning or sensation that they were about to pass out). This category can sometimes indicate cardiac/arrhythmic events, and a careful history and EKG interpretation are critical to determine if there are any high risk features.
Physical Examination and Tools
Perform a comprehensive physical exam including a neurological exam and heart sounds. Know what you are looking for on exam and what it could mean. Every syncope patient should also receive a 12 lead EKG, looking beyond ischemia to include signs of potential arrhythmias. Consider checking blood glucose levels, though a significant drop in glucose typically presents with persistent altered mental status rather than isolated syncope.
- Neurological exam– focal neurologic deficits are concerning for possible stroke, dissection, or intracranial hemorrhage as an etiology of the syncope.
- Heart sounds– A previously undiagnosed murmur is concerning for possible critical aortic stenosis, acute mitral valve failure, or hypertrophic cardiomyopathy as a possible etiology of the syncope.
- Lung sounds– Abnormal lung sounds suggests a possible hypoxic event as the etiology of the syncope such as CHF, pneumonia, or spontaneous pneumothorax.
- Abdominal exam– Abdominal tenderness or pulsatile mass is concerning for possible abdominal aortic aneurysm or ectopic pregnancy in the correct clinical setting.
- Extremity exam– unilateral swelling or calf pain is concerning for possible PE as the etiology of they syncope.
- EKG and telemetry monitoring during trasnport– any obvious arrhythmia or secondary signs of risk for possible transient arrhythmia are concerning for a transient arrhythmic event as the etiology of the syncope. It is important to monitor these patients on telemetry during transport to the hospital in case the arrhythmic event recurs you need to be ready to catch it.
The Role of EKG in Syncope
A 12 lead EKG is absolutely essential in assessing syncope. You’re looking for signs of arrhythmias or structural heart issues that could lead to syncope, such as AV blocks, Brugada syndrome, prolonged QT intervals, or signs of hypertrophic cardiomyopathy. There’s a range of subtle EKG findings that indicate serious cardiac issues, and familiarizing oneself with these patterns is essential for EMS providers.
For a more detail dive into the importance of the EKG in syncope, what you are looking for on the EKG and why, see the 7 can’t-miss ECG patterns blog post and the below infographic from emDOCs.net.
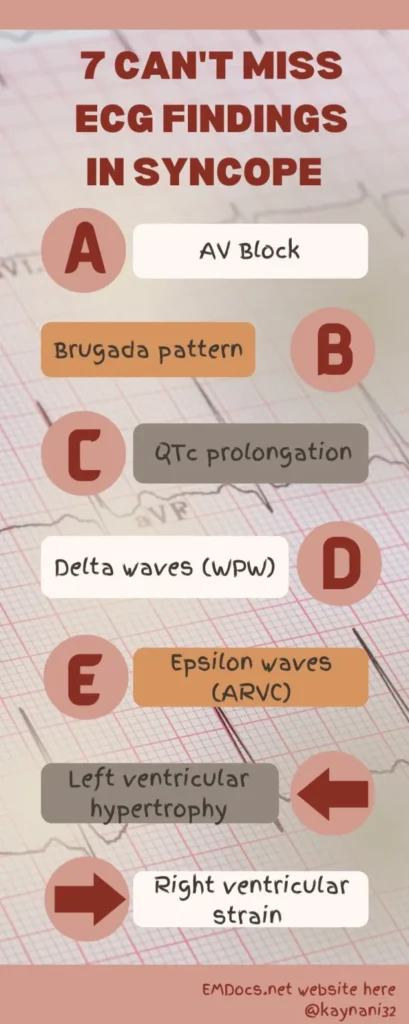
The only thing I would add to this list is the bifascicular block. If you see a bifascicular block in the setting of syncope or presyncope this is concerning for a developing trifascicular block which leads to a complete heart block and requires pacemaker insertion. See this post to learn more about the tifascicular block by life in the fast lane.
Risk Factors for Cardiac Etiology of the Syncope
- Patients with prior history of a cardiovascular condition such as atrial fibrillation, congestive heart failure, or myocardial infarction are at higher risk for a cardiac etiology of their syncope or near syncope.
- Syncope that occurred with exertion (climbing stairs, playing sports) or while seated/supine are at higher risk for a cardiac etiology of their syncope or near syncope.
- Any signs of heart failure, shock, or new murmur are at higher risk for a cardiac etiology of their syncope or near syncope.
Conclusion
In closing, syncope can range from a benign, self-limiting event to a harbinger of significant pathology. As EMS providers, understanding the potential causes and knowing how to perform a thorough assessment (most importantly what you are looking for on that physical exam) will help you differentiate between low risk and high risk, ensuring appropriate patient care and disposition.
Syncope may be common and is usually benign but is also simultaneously a high risk complaint. With enhanced knowledge and sharp clinical acumen, you can navigate this intricate challenge with confidence.
Learn More
Syncope in the Emergency Department: A Practical Approach
Arrhythmic syncope: From diagnosis to management
ACEP Policy on Evaluating Patients with Syncope in the Emergency Department
Emergency Medicine Cases Ep 172 Syncope Simplified with David Carr
ECG Pointers: 7 Can’t-Miss ECG Patterns of High-Risk Syncope – the “ABCDE Left Right” Mnemonic