326,000 out of hospital cardiac arrests are resuscitated by EMS annually. We know early high quality CPR increases survival. Hight quality CPR is defined by the AHA as:
- Chest compression fraction >80%
- Compression rate of 100-120/min
- Compression depth of at least 50 mm (2 inches) in adults and at least 1/3 the AP dimension of the chest in infants and children
- No excessive ventilation
With the advent of mechanical CPR devices like the AutoPulse and LUCAS, they promise consistency and endurance, attempting to mitigate human limitations such as fatigue and variability in compression quality. Many will tout the life saving capabilities of these mechanical devices. Yet, the question remains: do they truly offer a significant advantage over the well-established manual CPR method?
Enter the paper reviewed in this episode. Effectiveness of Mechanical Chest Compression Devices over Manual Cardiopulmonary Resuscitation: A Systematic Review with Meta-analysis and Trial Sequential Analysis by Sheraton et al published in the Western Journal of Emergency Medicine, July 2021.
The study conducted a detailed analysis of research data from 2000 to 2020, including randomized controlled trials (RCTs) and observational studies comparing mechanical CPR to manual CPR. The primary aim was to determine if mechanical CPR devices improve ROSC rates compared to manual CPR in out-of-hospital cardiac arrest situations.
The primary outcome they chose was ROSC sustained for >20min. While we know this is not a great patient centered outcome, the authors felt it would be the outcome most attributable to the CPR. Whereas, survival with good neuro outcome would be heavily influenced by variations in post-resuscitation care.
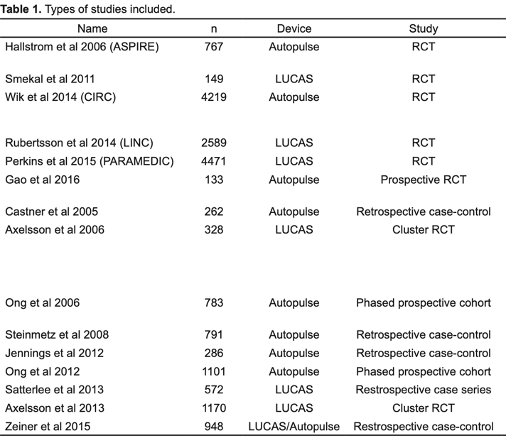
They identified 15 studies that met their inclusion criteria. 6 randomized controlled trials, 3 evaluating the LUCAS and 3 studying the Autopulse. 9 observational trials, 3 involving LUCAS, 5 involving Autopulse, 1 involving both LUCAS and Autopulse. For a total of 18,854 patients (LUCAS-10,227 / Autopulse-8,627).
Most observational studies were found to have a low or moderate risk of bias according to the new castle Ottawa scale (Appendix 1). As a reference a score of 8-9 is considered low risk and a score of 5-7 is considered moderate risk. The studies that had a comparably higher risk of bias in this group was mainly because they failed to control for any confounding factors by design, thereby losing out on the “comparability” score.
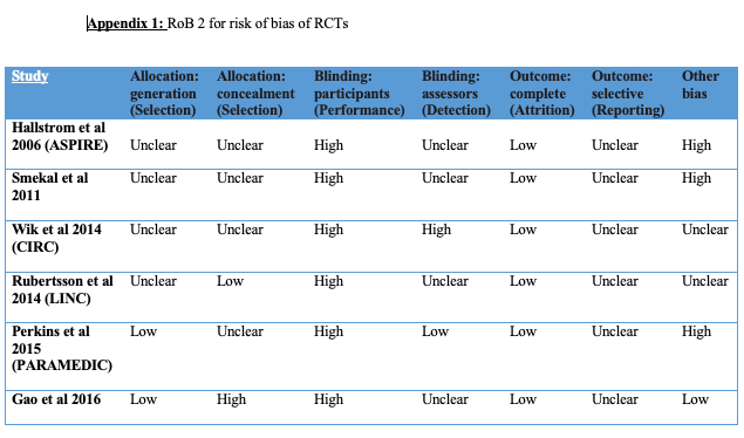
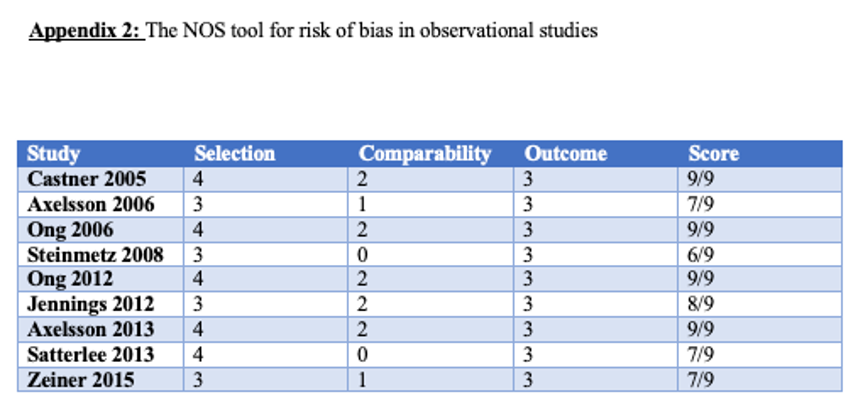
The RCTs, however, collectively had a higher risk of bias (Appendix 2). This is largely because randomized sequence generation was adequately performed in only two trials and allocation sequence concealment was adequate in only one. And given the nature of the intervention, blinding participants in the field is not possible, resulting in an increased performance bias in all studies. However, the PARAMEDIC trial did achieve a low assessor bias by blinding research nurses. Also noteworthy is that the ASPIRE trial had high “other” biases because it was stopped early due to interim evidence of worse outcomes in the intervention arm (mechanical CPR arm).
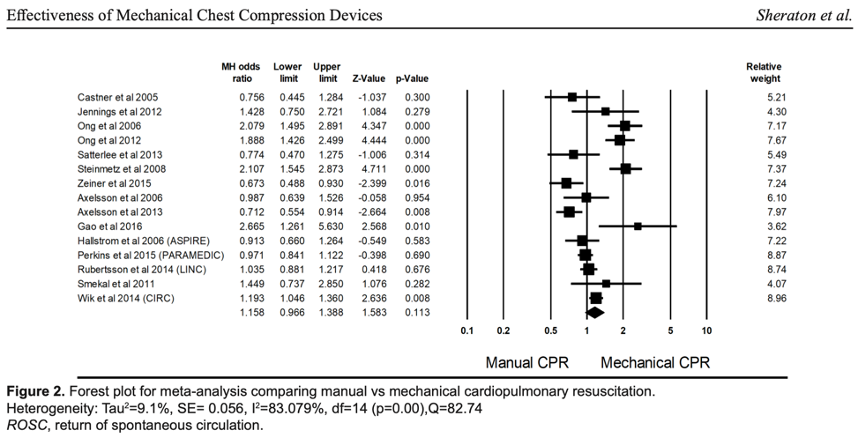
Meta-analysis summary statistics showed that mechanical chest compressions did not significantly improve ROSC (relative risk (RR) 0.80, 95% confidence interval (CI), 0.61, 1.04, P = 0.10; I2 = 65%) (Figure 2) when compared with manual chest compressions in patients undergoing resuscitation after OHCA (M–H odds ratio (OR) = 1.16, 95% CI, 0.97, 1.39, P = 0.11).
Multivariate meta-regression was performed to try to explain high between-studies variations in association between ROSC and mechanical vs manual CPR. Only three, achieved significance at the P <0.05, and these were- the percentage of witnessed OHCA, the percentage receiving bystander CPR, and time lag for EMS arrival. They found in these studies that as the percentage of those with witnessed OHCA and those receiving bystander CPR went up there was a decreasing benefit of mechanical over manual CPR for ROSC. However, the benefit of mechanical CPR over manual CPR increased with delays in EMS response. This suggests that mechanical CPR devices may have a place in non-ideal resuscitations where early initiation of quality CPR has not been possible.
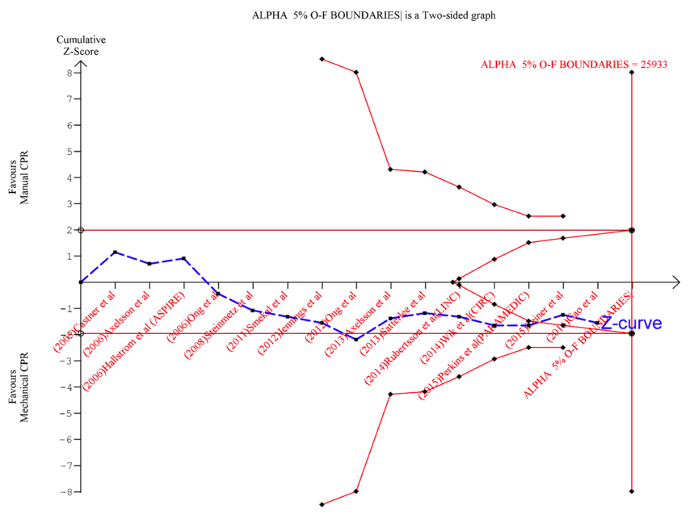
Finally they preformed a Trial sequential analysis which is a methodology that can be used in systematic reviews and meta-analyses to control random errors, and to assess whether further trials need to be conducted or whether there is sufficient evidence to make a determination and further studies would be unlikely to add to the current evidence base.
In the example above, vertical red line is required sample information size base on a power calculation, this takes into effect heterogenity. Green line is our standard cut off for determining statistical significance at our power calculation sample size. In the Trial Sequential Analysis software, trials are chronologically ordered, and interim analyses are conducted as each trial is added. As we can see in this example, the conventional meta-analysis crossed the convention significance boundary and would be reported as a positive trial, that the miquit intervention was statistically significant. However, the Trial Sequential Analysis software shows us that this finding is not sufficiently robust to reach a firm conclusion about miquit and it does so by using these monitoring boundaries. That’s because in an analysis where the ‘required information size’ has not been reached, the threshold for statistical significance must be inflated, using these monitoring boundaries, to account for sparse data; because the standard 95% confidence interval is not providing an adequate picture of the real uncertainty given the lack of sample size thus the cut-off for determining statistical significance must be below the usual p value of 0.05
Conversely, futility boundaries, are a threshold below which an intervention would be considered to have no clinically important effect and performing any further trials would be considered futile as the intervention does not possibly possess the postulated clinically minimally important effect
So as we can see in this example, although the conventional meta-analysis suggested, that the miquit intervention was statistically significant, the Trial Sequential Analysis software shows that this finding is not sufficiently robust and that further information is required before any firm conclusion can be reached about MiQuit efficacy. And when neither the monitoring boundaries nor the futility boundaries are crossed, further information is usually required.
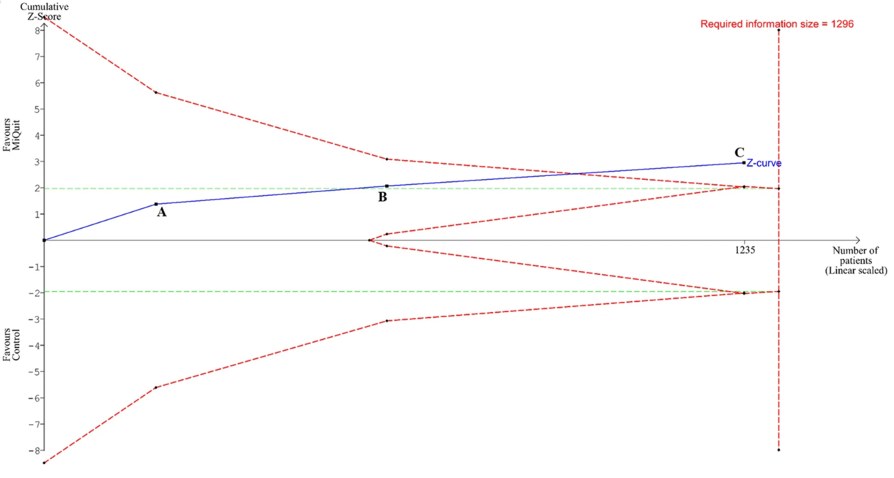
So we can see here that when we add trial C to the analysis although we did not quite reach our required information size, the effect was robust enough that it crosses the monitoring boundary and we can be firm in our belief that this is clinically significant.
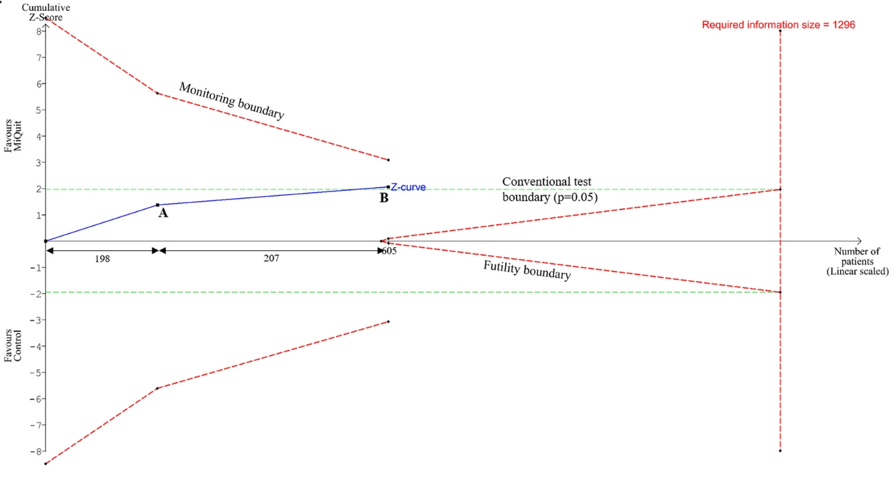
So now let’s look back at this studys analysis. We can see that based on the sample size we currently have and the effect or lack there of that has been shown across the trials we are now in a point of futility that further trials are unlikely to add or significantly change our current conclusion no matter their result. Trial sequential analysis suggested that sufficient evidence has already been accumulated to refute superiority of mechanical over manual compressions convincingly and that any further studies on this comparison would be futile to change that outcome.
This is when proponents of mechanical CPR with throw rotten tomatoes at us. Let us emphasize. This not saying that mechanical CPR doesn’t work. Mechanical CPR works. It works just as well as manual CPR. Just not any better. So in my mind it comes down to a resource question.
In fact, as previously mention, the authors in this paper performed what’s called a multivariate meta-regression analysis to determine if there was any signal of specific patient populations where mechanical CPR may be beneficial. They found that as the percentage of those with witnessed OHCA and those receiving bystander CPR went up, the benefit of mechanical CPR compared to manual CPR decreased. But as the time to EMS arrival went up, the benefit of mechanical CPR increased. Suggesting that mechanical CPR devices may have a beneficial place in non-ideal resuscitations where early initiation of quality CPR has not been possible.
If you work in a system where your percentage of witnessed CA and bystander CPR is low and your response times can be high, then mechanical CPR devices may be beneficial to your system. To me this describes many rural environments, whereas urban areas tend to have higher percentages of witnessed CA and bystander CPR and shorter response times.
The other system issues that play a deciding role in my mind that were not discussed in this paper include:
1. Do you have expendable cash to afford these devices? If so, great, they work just as well manual CPR and it frees up a provider from having to manually provide CPR. Which brings up my next consideration.
2. Do you have enough providers on scene to perform manual CPR? If you work in a system with limited manpower, mechanical CPR may be advantageous to free up providers on scene for other tasks.
3. Do you work in a system that routinely transports OHCA to the hospital and thus need to be able to perform CPR in a cramped moving vehicle with less hands?
I think these are all great reasons to utilize a mechanical device, just realize your outcomes are the same as with manual CPR. So if you work in a system with plenty of hands that doesn’t have the money to afford these devices or has alternative priorities they would like to use those financial resources for instead, you shouldn’t feel like you are providing suboptimal care by not having a mechanical CPR device. The outcomes are just as good with manual CPR and you can save the money for something else your system really needs.
Other FOAMed- CPR in Out of Hospital Cardiac Arrest: Man vs Machine