Anaphylaxis is a life-threatening condition that requires swift and effective management to prevent fatal outcomes. In emergency medical settings, ensuring aggressive and timely care can reverse the rapid progression of this disease. Today, we’ll delve into the AMAX 4 framework for treating severe, unresponsive anaphylactic patients, as shared by Bruce Hoffman, a senior educator at FlightBridgeED.
What is Anaphylaxis?
Anaphylaxis is defined as a serious systemic hypersensitivity reaction that is usually rapid in onset and may cause death. It involves the immune system’s IgE mediated excessive reaction to allergens such as bee stings, latex, foods like peanuts, shellfish, and more.
Severe anaphylaxis is characterized by potentially life threatening compromise in breathing and or the circulation, and may occur without typical skin features or circulatory shock being present. According to the 2019 World Anaphylaxis Organization, anaphylaxis is highly likely when one of the following two criteria are met.
For more from this article from 2019 that lays out this criteria and definition.
Pathophysiology of Anaphylaxis?
Anaphylaxis is an IgE mediated immune response.
What does that mean? Antigens are foreign materials the body responds to when it comes in contact to them by forming antibodies against the antigen in order to prevent it from causing any harm. Unfortunately, in this setting of anaphylaxis, IgE antibodies have been inappropriately built up after an exposure to certain usually benign antigens. Most common examples being bee stings, latex, and foods such as peanuts, shellfish, milk, eggs, soy, et cetera.
Upon re-exposure (so not the first exposure, the first exposure to the antigen, antibodies get built up, second and subsequent exposures, the antibodies go haywire) to the antigen, the IgE that has been built up leads to an exaggerated response and rapid mass release of chemical mediators from basophils and mast cells.
This mass release of chemical mediators includes histamine, triptase, and others. These chemical mediators then trigger a cascade of events that produce metabolites like prostaglandin D, leukotrienes and platelet activation factor. Let’s break down what each one of these does and how that produces what we see in anaphylaxis.
Histamine- increases vascular permeability and vasodilation leading to the swelling and hypoperfusion we see.
Prostaglandin D- functions as a bronchoconstrictor and also potentiates the peripheral vasodilation.
Leukotrienes and platelet activation factor- add to the bronchoconstriction and vascular permeability and also induce airway remodeling.
As you can see together, these lead to the swelling of the airway, Bronchoconstriction of the lungs and hypotension that we see in anaphylaxis. These are the vital ABCs. So it’s no surprise that the management of anaphylaxis relies on addressing these EMS core principles, ABCs.
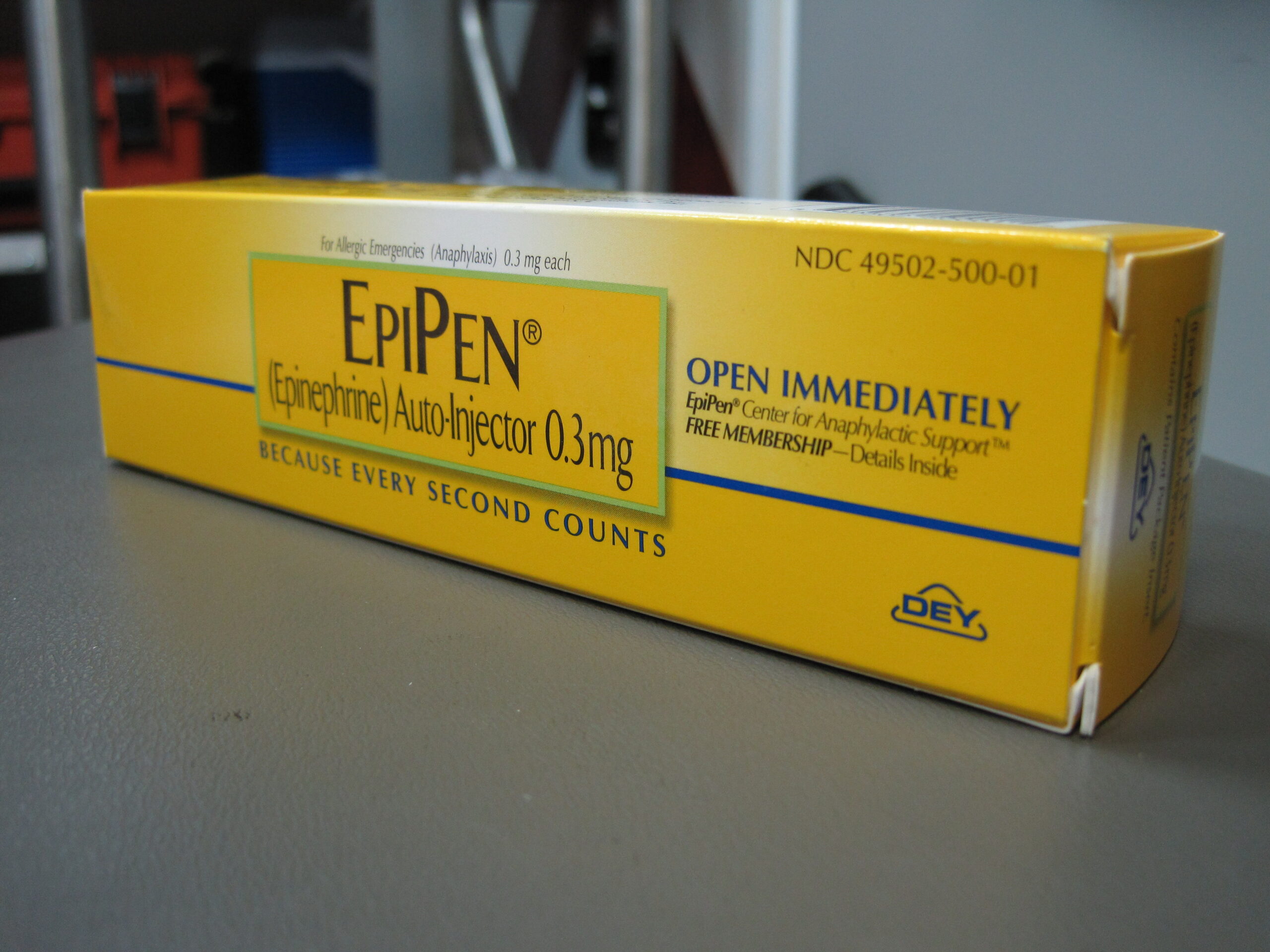
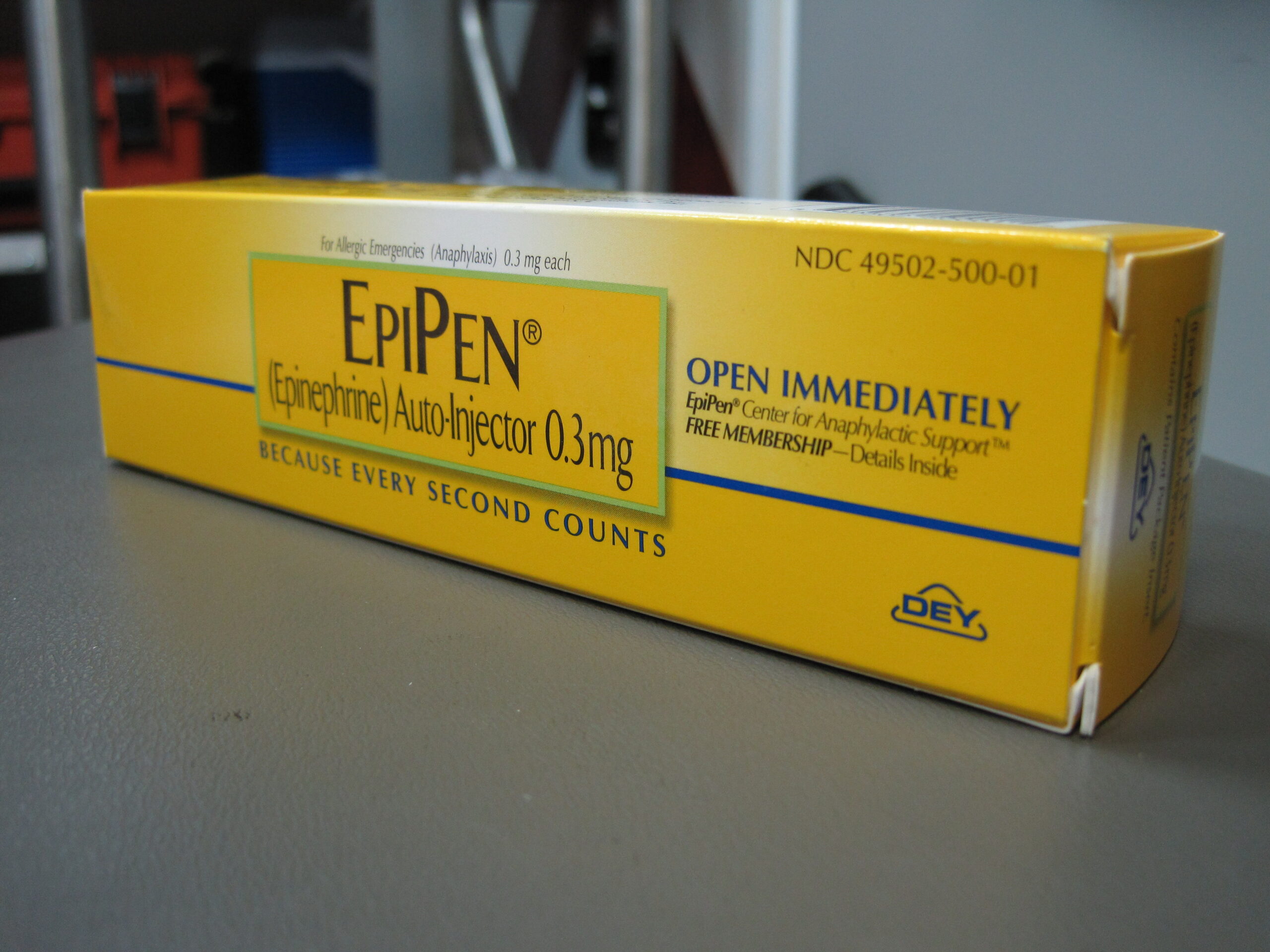
This is what we’re going to fall back on when we recognize and treat these patients. The good news is that epinephrine reverses all of this. Epinephrine will decrease permeability. Increase vascular squeeze and tone and cause bronchodilation. The adult dose is 0.3-0.5 mg of 1:1000 intramuscular epinephrine. That can be repeated every five to 10 minutes until you see effect. Intramuscular is preferred because studies have shown it leads to a more rapid delivery and produces better outcomes than subcutaneous or intravenous delivery.
If the patient is not improving after two doses of intramuscular epi, you may consider an IV push of 0.05 to 0.1 mg of the 1 to 10 cardiac code dose epi. So that’s going to be a 0.5 ml to 1 ml of the cardiac dose epi IV push and followed by a drip if the symptoms are still persisting despite this.
Adjunct therapy such as Benadryl, Bronchodilators, steroids may be provided as well, but none of these are going to save the patient’s life.
Let me repeat this, Benadryl will not save the patient’s life. Benadryl is an antihistaminergic, but does not address the other chemical mediators and so will not, and has never been shown to reverse anaphylaxis. It is merely a symptom adjunct Benadryl, bronchodilators, and steroids should not get in the way of administering Epi and administering it aggressively. Epi is the true life saving medication and should be your primary focus. Add in these others only when you’ve already treated appropriately with epinephrine.
For more information: https://www.ncbi.nlm.nih.gov/books/NBK482124/
When to Give Epinephrine in Anaphylaxis?
Multiple studies have shown that providers often wait too long before giving epinephrine and the rapid benefit of epinephrine in anaphylaxis far outweighs the risks of withholding the treatment. Part of this is our tendency to just complicate and overthink this decision. So let’s simplify this decision.
First and foremost, forget the allergist definition that anaphylaxis is any allergic reaction that involves two or more systems. This is vague, somewhat subjective, and just not useful to me as an emergency provider. My emergency definition of anaphylaxis, (i. e. when I’m reaching for epinephrine) does it involve any of the ABCs?
Airway- Is there airway involvement? Do they have any lip swelling, tongue swelling, posterior oropharyngeal swelling, or strider?
Breathing- Is there any difficulty breathing? Are they having to use accessory muscles? Is there wheezing?
Circulation- Are they hypotensive? Are there any signs of hypoperfusion?
It’s as simple as that. An allergic reaction that involves the ABCs is your hard stop. Absolutely 1000 percent give epi, no questions asked.
First Principle:
ABCs and anaphylaxis = life threat = equals aggressive anaphylactic treatment until the ABC symptoms are reversed.
Now, don’t get me wrong, a patient with an allergic reaction presenting with a rash and some GI upset should still be taken seriously. They need close monitoring to assure that they don’t develop any worsening symptoms. Do not blow these patients off. They are at risk for developing involvement of the ABCs and we can’t predict who will progress and who won’t. If they do progress to involve the ABCs, they will require the same aggressive treatment with epinephrine.
Caveat, if you have a patient with a known allergy, classic hives and severe abdominal cramping, or multiple episodes of vomiting, give this patient epinephrine, it’s going to reverse the process and make them feel a lot better. This is technically anaphylaxis. Just don’t let trying to decipher if this amount of vomiting or cramping counts make you forget about the ABCs. The most important point I can get across is, hard stop, if ABC involvement in the setting of an allergen exposure, give Epi without thinking twice.
How about if their throat is a little itchy? Does this count as involving the airway? This again becomes a little more subjective and this is again when I argue, use your brain. Certainly I don’t want to discourage you from treating with IM Epi in this situation. Many physicians I know will give epinephrine for a scratchy throat every time. But for me, it’s a little more nuanced. If it’s a 22 year old with a history of an anaphylactic nut allergy, who just accidentally ingested a nut containing product, give Epi to that person, even if it’s just a scratchy throat.
This is a high risk patient with a high risk pretest probability for severe anaphylaxis and a low risk for adverse event from epinephrine. Conversely, if it’s a 66 year old with a prior history of coronary artery disease and no known prior anaphylaxis with no known exposure, but a rash and an itchy throat, this is maybe still a high risk patient, but a lower pretest probability for severe anaphylaxis and a higher risk for adverse event from epi.
Maybe have the epinephrine nearby and definitely monitor closely for any objective signs of airway involvement or breathing or circulation.
Looking at the forest through the trees. Remember any allergic reaction with objective involvement of the ABCs. Do not pass go, do not worry about cardiac risk factors, give the epinephrine without a second thought. When in doubt error on the side of treatment, but if it’s subjective signs, like a report of a scratchy throat or mild nausea, and there’s no objective oropharyngeal swelling, no strider, their breathing is comfortable and their blood pressure is normal, then use your brain and assess their risk and pre test probability. And regardless of what you decide, monitor them very closely for progression of symptoms or ABC involvement.
The AMAX 4 Framework
The AMAX 4 framework was developed to address the needs of critically ill anaphylactic or asthmatic patients who have become unresponsive. Here’s a breakdown of its components:
A – Adrenaline (Epinephrine)
IV epinephrine is administered every 30 seconds until there is an improvement in the patient’s condition. Dose is 1 mcg/kg up to cardiac arrest dose. This aggressive dosing is crucial for reversing severe symptoms quickly and stabilizing the patient.
M – Muscle Relaxant
Rapid Sequence Intubation (RSI) is used if available to ensure that the initial attempt at securing the airway is successful. Muscle relaxants are administered to aid in this process, making the first intubation attempt the best attempt.
A – Airway Management
The focus is on definitive airway management. Given the severe bronchoconstriction in these patients, traditional supraglottic airways like iGel tubes are not sufficient. Endotracheal intubation or, if necessary, a surgical cricothyroidotomy is performed to secure the airway.
X – Extreme Management
This involves extreme and aggressive management of the patient’s hypoxia and other symptoms. From administering IV epinephrine to using other adjunct therapies like bronchodilators and vasopressors, the goal is to stabilize the patient within a critical four-minute window.
4 – Four Minutes
The framework emphasizes the urgency of reversing the patient’s severe symptoms within four minutes to prevent irreversible hypoxic brain injury. This tight timeline necessitates swift action and aggressive intervention.
Implementing the AMAX 4 Framework
Aggressive treatment of anaphylaxis is essential when standard measures fail. Here’s a step-by-step guide based on the AMAX 4 framework:
-
-
- Initial Epinephrine Administration:
- Initial dose upon arrival at the patients side should be intramuscular epinephrine (0.3 to 0.5 mg in adults, 0.15 mg in pediatrics) as it can be delivered immediately without waiting for IV access.
-
- If the patient is unconscious and IV access is available, dosing should be 1 mcg/kg every 30 seconds up to a cardiac arrest dose or until reversal of symptoms is achieved.
- Initial Epinephrine Administration:
-
- Assess and Manage Airway:
- Perform RSI with muscle relaxants if the patient is unresponsive.
-
- Secure the airway with an endotracheal tube; move to surgical cricothyroidotomy if intubation fails.
- Assess and Manage Airway:
-
- Extreme Measures:
- Continue aggressive IV epinephrine every 30 seconds.
- Use adjunct therapies like bronchodilators, steroids, and antihistamines as needed.
- Provide vasopressor support to maintain hemodynamic stability.
- Use high peak ventilatory pressures to overcome the patients bronchoconstriction and remember to allow for exhalation to prevent air trapping.
-
- Perform all of the above within 4 minutes.
- Extreme Measures:
-
- Monitor Closely:
- Ensure continuous evaluation of the patient’s airway, breathing, and circulation.
-
- Be ready to modify the treatment based on the patient’s response and evolving condition.
- Monitor Closely:
Conclusion
Anaphylaxis is challenging but highly treatable with the right approach. The AMAX 4 framework provides a structured method for aggressive management in the unresponsive anaphylactic patient, crucial for saving lives in critical situations. By understanding and implementing this framework, medical providers can ensure they are prepared to handle severe anaphylactic emergencies effectively.
For more information about the AMAX 4 framework and the story of its development, check out: https://www.amax4.org/algorithm.
Thank you for your dedication to saving lives, and remember, in the face of anaphylaxis, be swift, be prepared, and be aggressive