Podcast: Matt Mendes MD NR–P, Ross Orpet MD NR–P, Maria Moreira MD FACEP
Show Notes: Tyler Prince M4 NR–P
Ep. 3 Penetrating Neck Wounds
Penetrating neck wounds have the potential to injure many key structures. We discussed these injuries with all-around EM expert Maria “The Hammer” Moreira, MD. This episode is rife with pearls and deserves a thorough listen.
Anatomy
- Portions of many body systems pass through the neck
- Neurologic: spinal cord
- Respiratory: trachea, apices of lungs
- Cardiovascular: carotid arteries, jugular veins, vertebral and subclavian vessels
- Gastrointestinal: esophagus
- Structures not in the neck can be involved depending on trajectory of wound
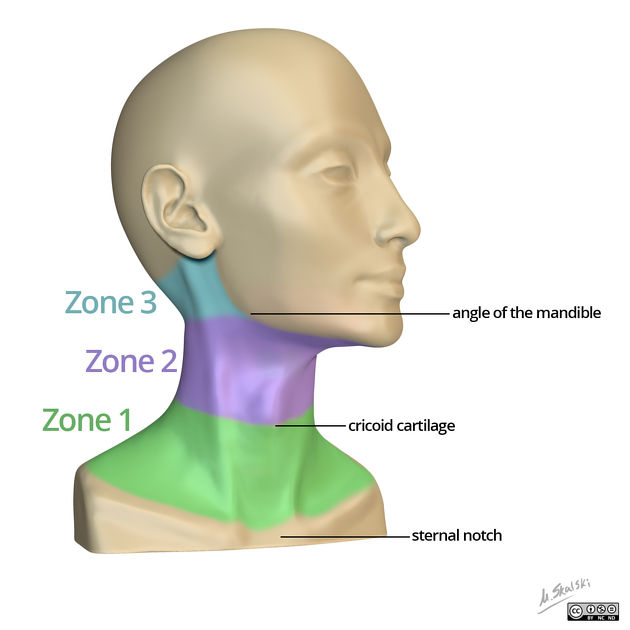
- Zone 1 wounds are most likely to involve thoracic structures
- Zones of the neck:
Clinical Presentation
- Evaluate penetrating neck wounds by system
- Respiratory
- Subjective: shortness of breath
- Objective: work of breathing, asymmetric lung sounds, stridor, crepitus
- Circulatory
- If present, hypotension/tachycardia are most likely due to hemorrhagic shock
- Expanding hematoma to neck
- Also consider possibility of tension pneumothorax and cardiac tamponade
- Neuro
- Consider neurogenic shock if not responding to fluids
- Evaluate for neuro deficits
- Take note of the zone(s) of the wound and report to receiving facility
Management
- Airway and Breathing
- First order of business in penetrating neck wounds
- “Airway” does not mean “intubate.” BLS options may provide an excellent temporizing measure. These patients are likely to have very difficult airways.
- Consider intubation patients who can’t manage their own airway: snoring, gurgling, poorly controlled secretions, persistent hypoxia
- Consider the risks of intubating: hypotension, hypoxia, acidosis (The HOP Killers “EMCrit: The Laryngoscope as a Murder Weapon series”)
- Preoxygenate prior to intubation
- Address hypotension prior to intubation
- Consider tension pneumothorax and cardiac tamponade; correct prior to intubation if possible
- Be ready to do a cric! Can’t intubate, can’t oxygenate = CRIC
- Circulation
- Do not explore/probe neck wounds!
- Provide direct pressure to open wounds throughout the entire call—may have fire or other first responder ride in and assume this role
- Hemorrhagic shock: bilateral large bore IVs, blood products vs crystalloids
- If tension pneumothorax is suspected, perform needle decompression prior to intubation
- Disability
- C-collars should be used only if a neuro deficit is present
- Chance of C-spine injury in penetrating neck trauma is low
- 1.35% c-spine injury in GSWs to neck
- 0.12% c-spine injury in stabbings to neck
- Actual spinal cord injury rates are even lower
- Open collars and visualize the neck!
- Definitive management throughout history
- Defunct methods
- Expectant management: 35% mortality
- By zone:
- Zone 1 = imaging
- Zone 2 = surgical exploration
- Zone 3 = imaging
- Modern approach: “no zone”
- “Hard signs” = OR emergently for surgical exploration
- Hemodynamically unstable
- Expanding hematoma or severe hemorrhage
- Neuro deficits
- Thrills or bruits
- Absent radial pulse
- Air bubbling from wound
- Massive hemoptysis or respiratory distress
- Soft signs = Imaging (CT angiography) to guide management
- Mild hypotension
- Minor hemoptysis
- Subcutaneous air
- Non-expanding hematoma
- Dysphonia or dysphagia
- If asymptomatic with platysma violation = observation 24 hours in order to monitor for the development of hard or soft signs.
- If the platysma is intact, chance of damage to key structures is extremely low.
- “Hard signs” = OR emergently for surgical exploration
- Defunct methods
Takeaways
- The neck contains key structures including the trachea, major vasculature, spinal cord, esophagus, and the apices of the lungs.
- Penetrating neck wounds should be approached in respect to the ABCs:
- Airway/Breathing: intubate if necessary, but consider basic airway management. BLS adjuncts are an excellent temporizing measure permitting resuscitation before intubation. These patients will have difficult airways. Provide oxygen and ventilate as needed. Remember- can’t intubate, can’t oxygenate = CRIC.
- Circulation: direct pressure is key to stop bleeding. If these patients are in shock, it’s most likely due to hemorrhage. That being said, you should still consider tension pneumothorax and decompress if necessary.
- Disability/Exposure: A C-collar should only be used if neuro deficits are present. Be sure to visualize the entire neck—remove the collar, if placed prior to your arrival, in order to inspect wounds.
- Hospital management will involve stabilization followed by either emergent surgery or CT scan to better visualize anatomy. If the platysma is violated, patients should at a bare minimum be observed for 24 hours.
Resources
https://rebelem.com/penetrating-neck-injuries/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5849205/
https://www.entnet.org/sites/default/files/Trauma-Chapter-7.pdf